When we get sick, we want our bodies to mount the best possible defense against invading pathogens. The immune system is responsible for fighting infections. Researchers at Boston’s Children’s Hospital have discovered that oxPAPC, a chemical that naturally occurs in damaged tissues, triggers a strengthened immune response that could have useful implications for developing more effective vaccines. The specific cells that oxPAPC activates are dendritic cells.
Dendritic cells provide a screening mechanism for antigens present in the body. Self-antigens, like dead cells and proteins, are usually not a threat. However, foreign antigens, like outside bacteria, can be harmful. The dendritic cells ingest the antigens through endocytosis and present the fragments to T-cells.
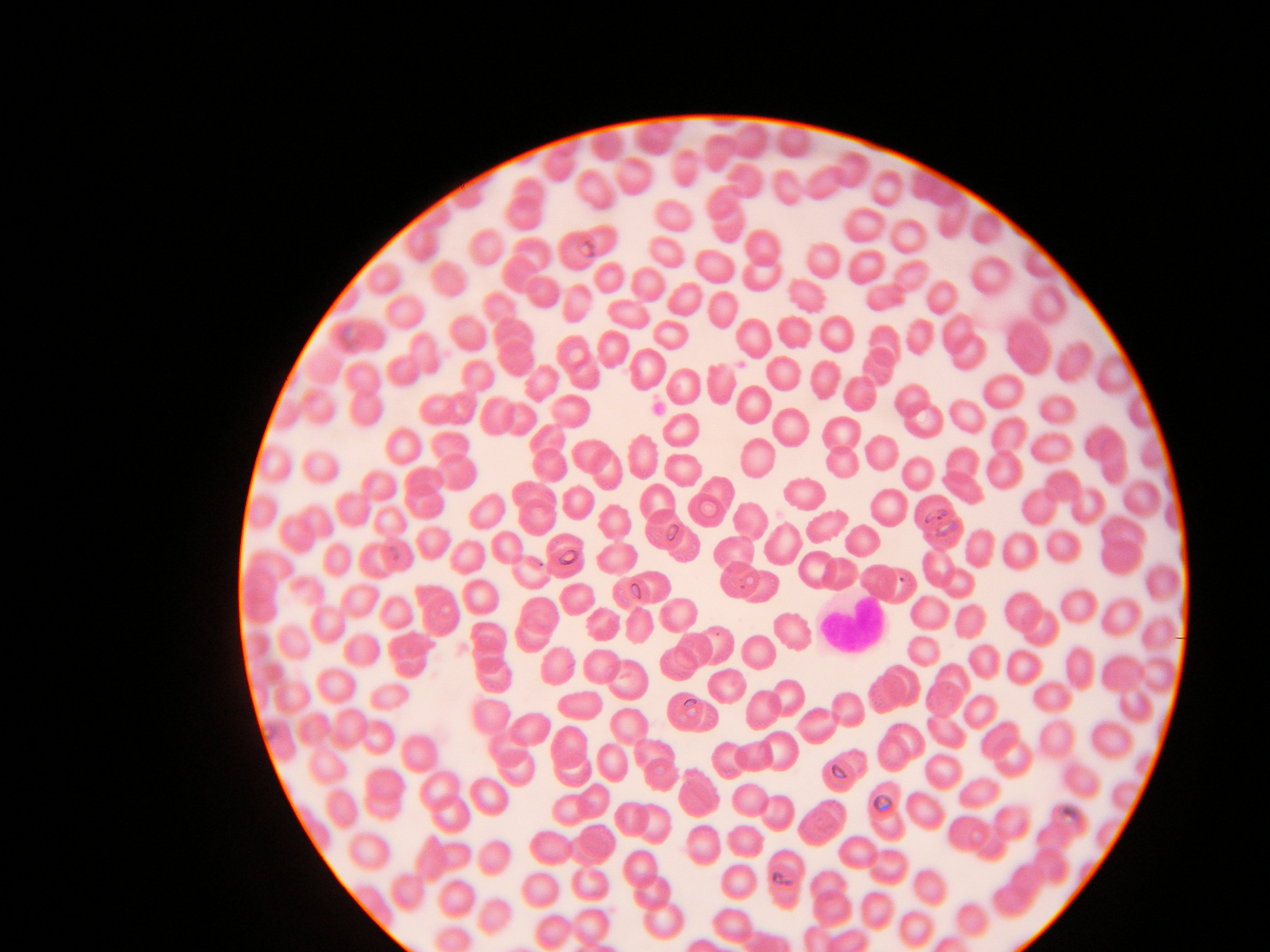
T cells are a type of white blood cell and part of the body’s immune system. Different T-cells have receptors which recognize different antigens and destroy them. In the case of foreign antigens, the dendritic cells present both the antigen fragments and a second stimulatory molecule to the T-cell, resulting in an immune response by the T-cells against the foreign antigen. When the dendritic cells present T-cells with a self-antigen, they neglect to include the second stimulatory molecule. Without this second signal, the T-cells divide for a short time but eventually kill themselves in a process called apoptosis. The eradication of T-cells targeted towards the self-antigen causes the body to develop a tolerance for it since there are no longer any cells in the body that can target and destroy that antigen. This is a helpful mechanism that prevents our bodies from attacking its own self-antigens.
Image Source: Sciencefoto.De – Dr. Andre Kempe
In mice, researchers have shown that the presence of oxPAPC resulted in an immune response five times greater than the response without oxPAPC, meaning increased T-cell activation in response to an antigen. This is due to the ‘hyperactive’ state that is induced in dendritic cells following exposure to oxPAPC. The specific enzyme targeted is caspase-11, which promotes hyper-activation in dendritic cells when in the presence of oxPAPC. Hyperactive dendritic cells live longer, are better activators of T-cells, and have been shown in mice to strongly activate memory T-cells, or cells which have previously been exposed to their target antigen and are thus more effective at combating pathogens than regular T-cells.
This discovery could lead to the development of improved vaccines. Using oxPAPC to trigger a stronger immune response to vaccines would better equip the body’s immune system to fight that same disease if encountered in the wild. The researchers intend to test oxPAPC in clinical trials.
Feature Image Source: Heart-shaped White blood cell by La Melodie