A potential new tool in the ongoing fight against Ebola has been developed by researchers at Harvard, and it fits on a piece of paper. Dr. James Collins, who led one of the teams involved in designing the system, described it as an “in vitro, sterile, abiotic operating system upon which we can rationally design synthetic, biological mechanisms to carry out specific functions.”
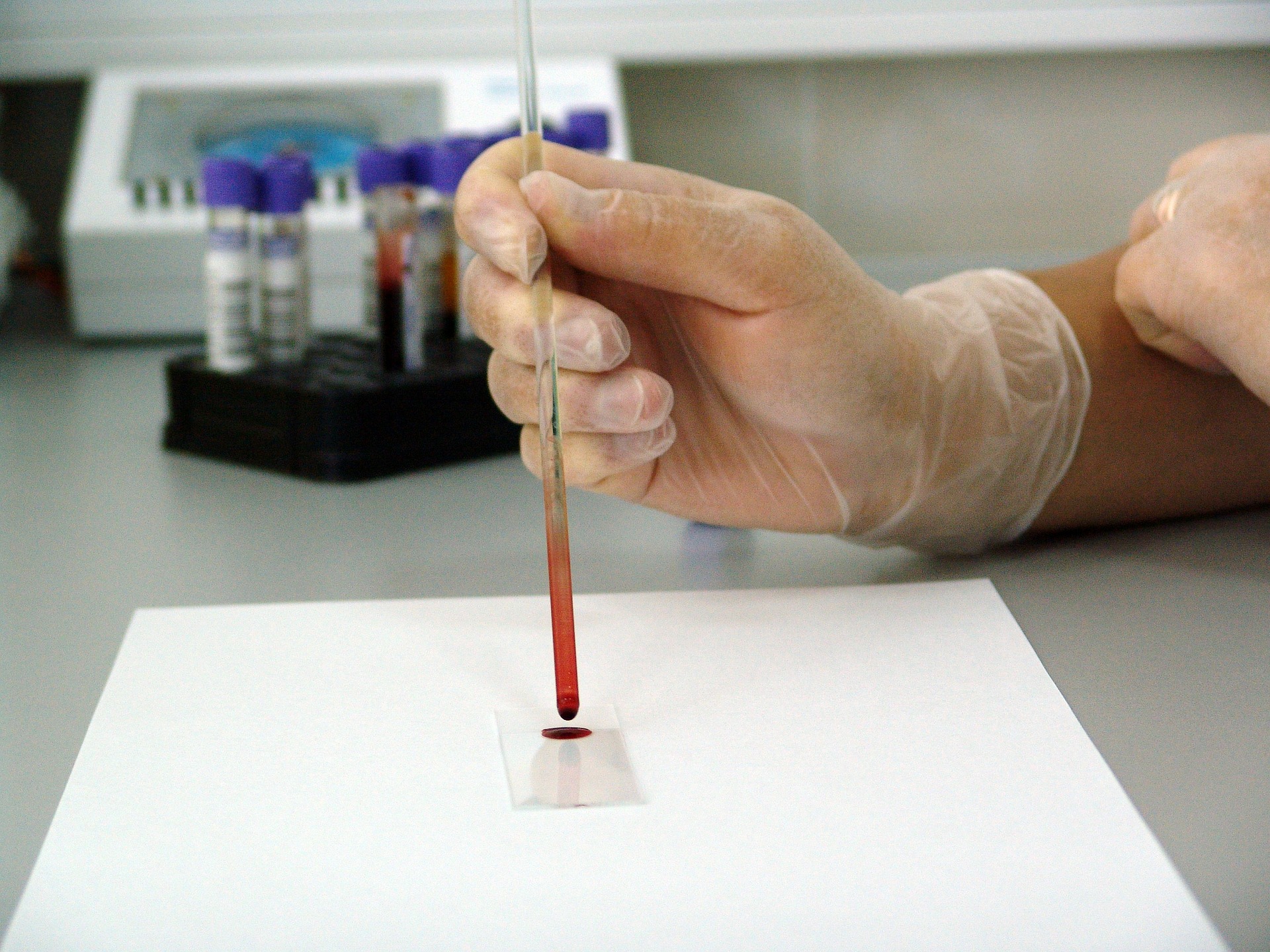
These synthetic gene networks are designed to interact with specific viral or bacterial RNA strands and can be designed to match specific strains of diseases like Ebola. Blood samples of Ebola patients contain RNA that codes for viral proteins essential to Ebola’s ability to replicate and infect. Whenever those RNA molecules are isolated, scientists can design a biosensor matched to that RNA to detect that particular viral protein. The interaction causes a fluorescent protein to change the color of the biosensor, providing a visual indication identifying RNA sequences. The pattern of activation in the array can tell scientists what the blood is contaminated with. A prototype biosensor was able to differentiate between Sudan and Zaire strains of the Ebola virus within an hour.
These paper-based diagnostic systems can be freeze-dried and shipped across the world for use in the field as well as provide rapid diagnostics in the laboratory. Once freeze-dried, the sensors are effective for a year, ready to use after rehydration with water.
Lifesaving Blood
Several prospective therapies are being developed to combat the disease. A common ingredient and source of therapeutic material is the blood of Ebola survivors. This blood contains antibodies against the Ebola virus, which are able to spur the immune system of an infected patient and may be able to confer resistance to the uninfected. By isolating antibodies that appear to be effective in hindering the viral life cycle, researchers can develop drugs to treat Ebola. One such experimental drug, ZMapp, was able to cure 100% of infected rhesus monkeys in a controlled study. Although it has been used in seven human cases, of which five survived, it is unclear how much of a role the drug played. Mapp BioPharmaceutical, a San Diego biotech company, formulated ZMapp in January 2014. It is composed of three antibodies, grown in tobacco plants for one week before purification. It was made in limited supply for animal testing, but Mapp provided the drug free of charge to Ebola patients until the supply was exhausted on August 12. Scientists are looking into several antibodies that may have a therapeutic effect.
The National Institute of Health announced an experimental vaccine that was co-produced by the National Institute of Allergy and Infectious Disease (NIAID) and GlaxoSmithKline (GSK). The vaccine contains genetic material from both Sudan and Zaire strains of Ebola, housed in a carrier virus known as cAd 3 (chimpanzee-derived adenovirus 3). Although cAd 3 gives chimps a cold, the virus doesn’t make humans sick. In Phase 1 clinical trials, the vaccine prompted antibody production in all 20 study participants. Researchers also observed elevated levels of CD8 T cells, immune system cells that may mediate immunity, in several of the subjects. The vaccine is undergoing additional trials to pass Phase 1.
Another experimental vaccine has been developed by the Public Health Agency of Canada’s National Microbiology Laboratory. It utilizes a vesicular stomatitis virus as a carrier for the Ebola material. Several clinical trials are underway in the United States, Switzerland, and Nova Scotia, with results expected as early as this month.
Fighting More than the Virus
Ebola clinics in Africa need all the help they can get. If these paper sensors are mass produced and shipped to Africa, they could greatly reduce the amount of time required to analyze a blood sample for Ebola, saving time and money for healthcare workers in Africa. Most clinics contain two patient isolation areas, one for “suspect” Ebola cases and one for “confirmed” cases, to reduce the risk of spreading infection. Faster lab work would reduce the time patients spend in the suspect area, reducing the risk of infection, and opening space for other patients.
Logistics represent a large burden for clinics that often provide their own electricity through generators and maintain stockpiles of chlorinated water (0.50% for sanitizing, 0.05% for handwashing) in places that often don’t have municipal utilities. In one clinic in Freetown, Sierra Leone goes through 200 sets of personal protective equipment daily, including boots, scrubs, gloves, coveralls, respirators, hoods, aprons, and goggles. Once used, all of this equipment must be sanitized and safely disposed of. Although the development process for these sensors will take some time, cheaper and more efficient diagnostics may help clinics hold over until vaccines are available.