It was the early 1900s. Mrs. Davis, a 40 year old woman, suffered from epilepsy, a neurological disorder characterized by seizures. At the time, there was a prevailing medical view that there was a relationship between epilepsy and the uterus of a woman. Now, as bizarre as this idea might seem to you and me, her surgeon at the time, Dr. Pratt, took this idea very seriously.
Mrs. Davis was put under anesthesia as soon as she arrived at the hospital, and what had initially seemed to be merely a medical follow-up somehow ended up leading up to a surgery that she did not remember ever giving consent for.
And on that fateful day, in the recovery room, this 40-year-old later woke up to learn that her uterus and ovaries were now gone. These events consequently led to the Pratt vs. Davis Supreme Court case of 1906. The Supreme Court ruled that since Mrs. Davis’s surgery was performed without her consent, that this was an incidence of “intentional and unconsented touching” and was thus a case of battery.
This was, in fact, one of the earliest cases that propelled the world to see the importance of having an Informed Consent. Had an informed consent been required at that time, Mrs. Davis could have easily been saved from undergoing the surgery that day. But it was not until the 1970s that physicians were actually required to fully disclose to the patients the procedures they were going to perform on them and the risks and the benefits that these entailed.
Image Source: Peter Dazeley
But even today, patients still often have very meager awareness of the risks involved with a particular procedure, even after having signed the white consent form. This element sheds light on the unresolved issues that still plague our system. The strategies that have been suggested to improve patient understanding of the informed consent form include increasing the focus on shared decision-making, simplifying the information presented in these forms, and sufficiently training physicians regarding proper consent.
Simplification of the information has indeed proven to be quite effective. In fact, a study performed at the University of Texas found that making the consent form more easily comprehensible can drastically improve the understanding of the patients about the risks involved with their procedures.
But only a simplification will not be sufficient to resolve all the problems with this situation in the long run. As the number of people suffering from Alzheimer’s and other chronic diseases that impair decision-making capacities doubles in the next few decades, the struggle with consent in healthcare is only going to get more intense due to issues concerning incapacity and finding alternative decision makers. The success of the studies, such as the one mentioned before, serve to illuminate how only a few key changes will ultimately be enough for us to propel the reality of the current informed consent towards one day reaching our theoretical ideals in the future.
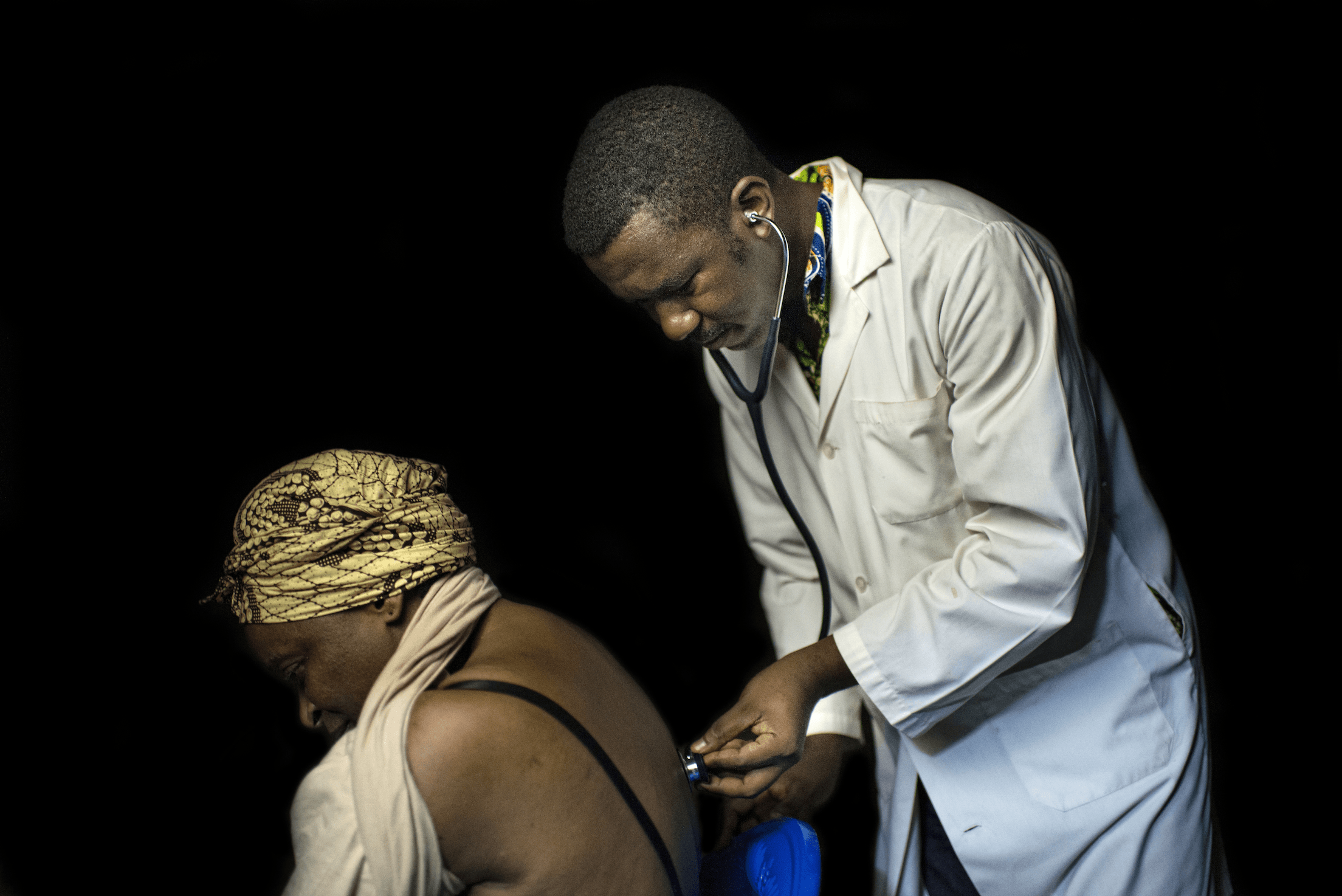
Feature Image Source: Doctor by CIFOR