In an earlier article, we discussed schizophrenia, a commonly misunderstood disease with negative connotations being placed on it due to various fallacies–so let’s get the facts straight. Impacting nearly 1% of the total human population, schizophrenia is a devastating mental illness that originates from impaired brain development that eventually leads to imbalanced signaling in the brain. This, in turn, is thought to cause the debilitating hallucinations and paranoia that these patients experience.
Research led by scientists from Duke-NUS Graduate Medical School Singapore, however, points out that they may have found the key to “cracking” schizophrenia by linking the abnormal behavior of two genes (BDNF and DTNBP1) to the underlying causes of schizophrenia.
Image Source: PeopleImages.com
Dr. Je analyzed signaling activity in cells that had lowered or nonexistent levels of the DTNBP1 gene since reduced levels and/or genetic disruptions of the DTNBP1 in mice resulted in schizophrenia-like behaviors. Using multiple model systems, Dr. Je and his team observed that low levels of DTNBP1 resulted in dysfunctional neural circuits and over-active neuronal network activity, as well as reduced levels of the secreted protein molecule, BDNF.
What is BDNF? Playing an important role in the interneurons’ ability to connect to the brain, BDNF was shown to be one of the most important factors that regulated the development of a normal brain circuit. How does this work, however? And what does DTNBP1 have to do with this? Turns out, interneurons receive BDNF via a transport system run by DTNBP1.
Confused? Imagine that BDNF is an important parcel and DTNBP1 is a delivery van driver. Without the driver, the important parcel cannot be properly sent to its destination. Without BDNF, the abnormal circuit development and brain network activity observed in schizophrenia occurs. Interestingly, however, Dr. Je discovered that when BDNF levels were restored, brain development and activity returned to normal levels, even with the absence of DTNBP1.
While the two genes DTNBP1 and BDNF have been singled out as risk genes for schizophrenia in studies before, this is the first study that shows that the two function together. Pinpointing the importance of the abnormal delivery of BDNF has shed considerable insight into how the brain network develops while also presenting possibilities for potential treatments for schizophrenia that are designed around enhancing BDNF levels.
So how will this help us out in the future? Dr. Je plans to organize a follow-up study to test whether these findings are viable in animal trials. If proven successful, correcting the imbalance within the brain circuits of schizophrenia patients through the angle of attack developed in this study could be the key to finding a cure.
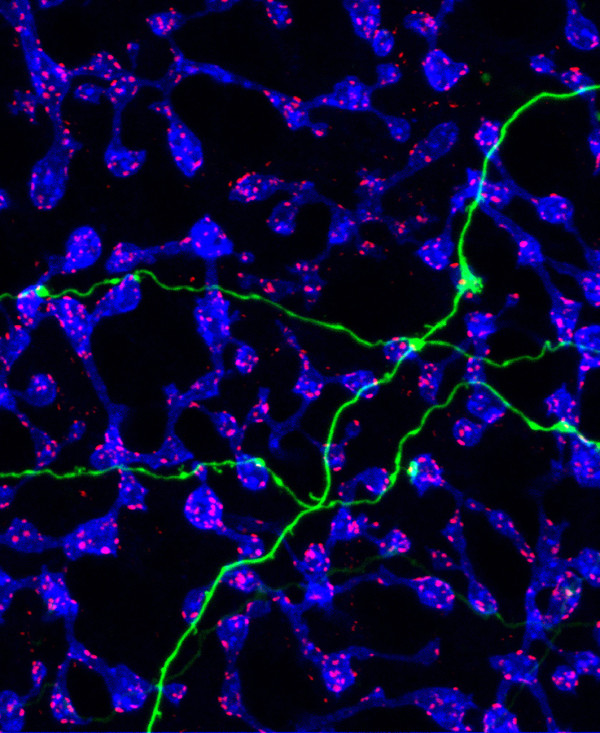
Feature Image Source: “Criss-Crossed Wiring in the Retina” by National Eye Institute is licensed under CC BY 2.0