A new breakthrough treatment for bacterial infections is here! Researchers have developed an artificial spleen capable of cleaning up bacteria-infected blood by using specialized beads to bind and remove floating bacteria in the blood.
Bacterial infections are usually treated with antibiotics, drugs that disrupt bacteria’s ability to survive. The first and most widely used antibiotic, discovered by Alexander Fleming, was penicillin, a wonder drug at the time, that treated most infections. The excessive use of antibiotics, however, has several serious consequences. Every time an antibiotic is used against bacteria, there is always a small chance a small population of bacteria may survive and develop resistance to that specific antibiotic. Further use of the same antibiotic would therefore have no effect on the surviving bacteria colonies. This is why most bacteria have developed resistance against penicillin. Widespread use of antibiotics has also led to the emergence of a scary phenomenon: superbugs (multidrug resistant bacteria, example: gonorrhea). These superbugs are extremely hard to cure with traditional antibiotics and require stronger antibiotics that may cause numerous side effects.
Image Source: Burger/Phanie
Another consequence of using antibiotics is the disruption of the body’s natural bacteria in the gut. Antibiotics are non-discriminate, meaning they kill of any bacteria that fits its profile, leading to an imbalance of helpful gut bacteria. These friendly bacteria are known to help people regulate hormone balance, metabolism, provide vitamins, and are essential contributors to health.
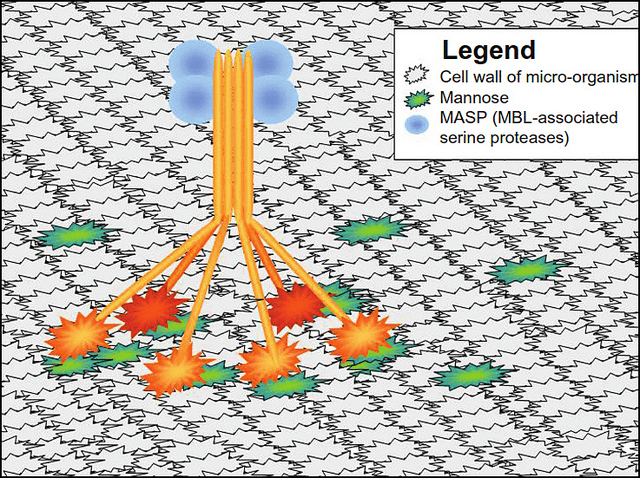
With the advent of this new treatment technique, the artificial spleen, a person suffering from bacterial infection can be hooked up to this filtration device and have their blood cleaned of pathogens and returned back into circulation. The key component of this device is the modified MBL (mannose-binding lectin) coated nano-beads. Normally MBLs are proteins that recognize common conserved bacterial surfaces (surfaces on bacteria that are the same for most bacteria), bind to them, signal to the body that they have detected bacteria, and activate the body’s immune system. The novelty of these modified MBLs is the removal of MBL’s ability to signal for immune activation. This means that the modified MBLs recognize a broad range of bacteria and can bind to them specifically, but do not activate the immune system. Because a system-wide activation of the immune system is known to cause sepsis, a whole body inflammation that can be fatal, we do not want the immune system to be overly activated. By removing the pathogens from the blood without activating the immune system, sepsis can be avoided, and beads can eventually be taken by a diagnostician and cultured to find out the nature of the infection.
So far the mice models look very promising. Compared to the control mice population’s survival rate of 14% (infected with E. coli or Staphylococcus aureus but untreated with artificial spleen), mice that received treatment had an 89% survival rate, a drastic improvement. When asked if the artificial spleen could handle treating a human (around five liters of blood), the scientists ran five liters of human blood mixed with bacteria and fungi on the device and found most pathogens removed after five hours. When combined with antibiotic treatment after running treatment through the artificial spleen, the patient could be cured of infection while limiting the possibility of bacteria developing resistance. If, however, patients were given just antibiotics from the start, then there are more bacteria to kill and a higher chance for some to survive and develop antibiotic resistance.
TL;DR: A new device, inspired by the spleen, filters and removes pathogens from the blood, drastically improving survival rate from infections.
Feature Image Source: Figure 3 by Libertas Academica