Autoimmune diseases occur when the body’s immune system, which defends the body against diseases and infections, instead attacks the body’s healthy cells. These diseases, including multiple sclerosis (MS), rheumatoid arthritis and type 1 diabetes, affect up to 50 million Americans, according to the American Autoimmune Related Diseases Association (AARDA). In fact, MS alone affects around 2.5 million people globally. Unfortunately, there are about 80 types of autoimmune diseases, and many have similar symptoms, making them harder to differentiate. As there is no known remedy for these diseases, treatment usually focuses on immunosuppression—medication that decreases the immune response or reduces immune system activity.
A new breakthrough has been found to fight these debilitating disorders.
Researchers at the University of Bristol have just discovered how cells convert from being aggressor cells (as in autoimmune disorders) to being protector cells against disease as they normally are. This study has been published in Nature Communications, and their research is paving the path to extensive use of antigen-specific immunotherapy for curing autoimmune disorders like MS.
Image Source: JGI/Jamie Grill
Scientists chose cells causing autoimmune disease, and attempted to reduce their damaging effects on healthy body tissues, as well as increase their capability to protect against disease. This cell conversion has already been applied to allergies, in a process known as “allergic desensitization“, but had not yet been applied to autoimmune disorders. The researchers showed how administering fragments of proteins that are normally attacked will lead to adjustment of the autoimmune response, also revealing that an effective cure is possible by slowly increasing the injected antigenic fragment dosage.
To study how immunotherapy works, the researchers probed inside immune cells to locate which genes and proteins were turned on or off during the treatment. They discovered alterations in gene expression that clarified how their effective cure led to conversion of aggressor cells into protector cells. The result was a reinstating of self-recognition, whereby the immune system disregarded its own healthy tissues, but remained armed to defend against disease or infection. This method of targeting faulty cells eliminates the necessity of immune suppression medications which have side effects like infections, development of tumors, and disruption of natural regulatory mechanisms.
Professor David Wraith, who led the research, said, “Insight into the molecular basis of antigen-specific immunotherapy opens up exciting new opportunities to enhance the selectivity of the approach while providing valuable markers with which to measure effective treatment. These findings have important implications for the many patients suffering from autoimmune conditions that are currently difficult to treat.”
This new research could improve the lives of millions by providing relief to those suffering from autoimmune disorders. The work is currently undergoing clinical development through the biotechnology company Apitope.
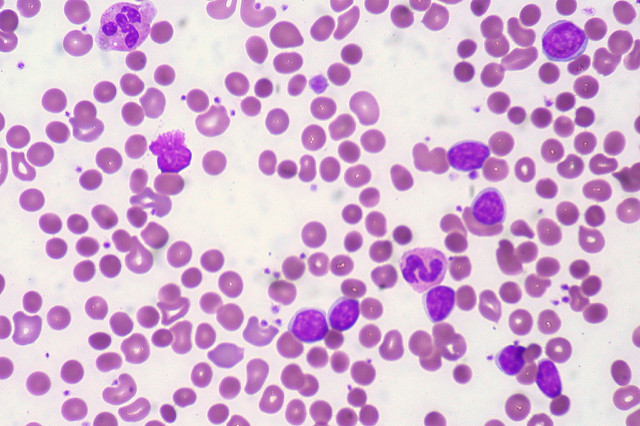
Feature Image Source: CLL with Autoimmune Hemolytic Anemia by Ed Uthman