The discovery of antibiotics has been revolutionary in terms of our ability to treat bacterial infections; however, not long after the initial discovery of antibiotics, some flaws became apparent. After a while, antibiotics were no longer working against infections that they were once successful in dealing with, a phenomenon known as antibiotic resistance. This can be explained, simply, by the evolutionary mechanism of natural selection, whereby bacteria that happen to be resistant to the specific antibiotic’s method of destruction or inhibition are able to survive and proliferate better than other bacteria. A similar but distinct concept that is relevant in this discussion is antibiotic tolerance. Tolerance results from the presence of a population of cells called persisters, which as their name suggests, remain intact and alive despite the introduction of antibiotics. Being able to treat bacterial infections is essential to maintaining the health and longevity of the human population. It is important, then, to develop tools for overcoming the challenges posed by both antibiotic resistance and tolerance. Fortunately, a recent study may provide a better understanding of the latter.
Image Source: Science Photo Library – MEHAU KULYK
Researchers have found that mycobacteria have varying degrees of responses to antibiotics based on size and time of division. Mycobacteria can cause tuberculosis, which can be fatal if untreated. In contrast to popular belief, the infection can only really spread through the air and not through other forms of physical contact. Although mycobacteria divide in a such a way that each daughter cell is genetically identical to the other, the researchers found that characteristics like their size and growth speed would often differ. Moreover, when researchers looked at the susceptibility of the bacteria to Rifampicin, an antibiotic used to treat tuberculosis, they found that larger bacteria were better able to tolerate the presence of the antibiotic. In addition, the researchers examined susceptibility in regards to timing of the cell cycle and found that bacteria in the middle of their cell cycle had more antibiotic tolerance than bacteria in the beginning or end of their cell cycle.
The results of this study by researchers from Tufts University may contribute to the development of antibiotics that are more effective at targeting persister cell populations that contribute to antibiotic tolerance. The study suggests that antibiotic development should take into account minute differences, such as size of the bacteria, in order to maximize treatment effectiveness. This is important because weak or inefficient antibiotics would essentially cause more harm than good by allowing surviving populations of bacteria to proliferate. Consequently, the ultimate goal of future antibiotics should be to eliminate all traces of invading bacteria. Being able to do so will serve as a crucial tool for achieving victory in the arms race against infectious bacteria. Until then, however, a better understanding of the unique attributes of bacterial cells that confer antibiotic tolerance will remain a goal for the scientific community.
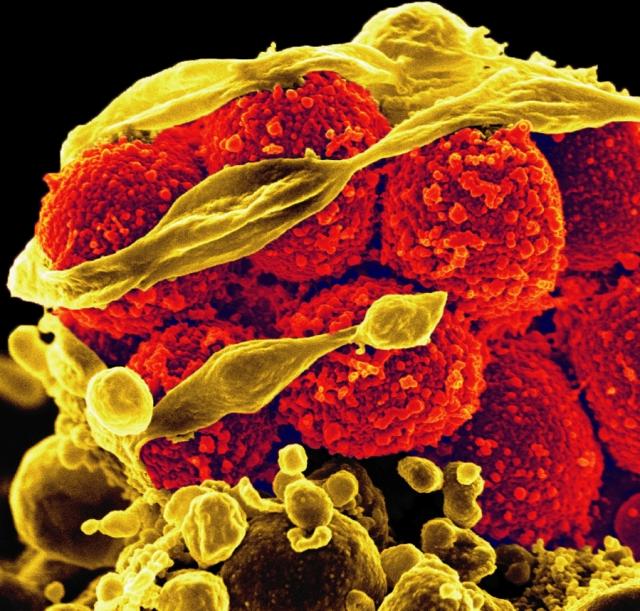
Feature Image Source: Methicillin-Resistant Staphylococcus aureus (MRSA) Bacteria by NIAID