 Author: Sopyda Yin
Author: Sopyda Yin
Editor: Samantha Yip
Graphic Editor: John Nguyen
Disclaimer: The following content will discuss on suicide and substance abuse.
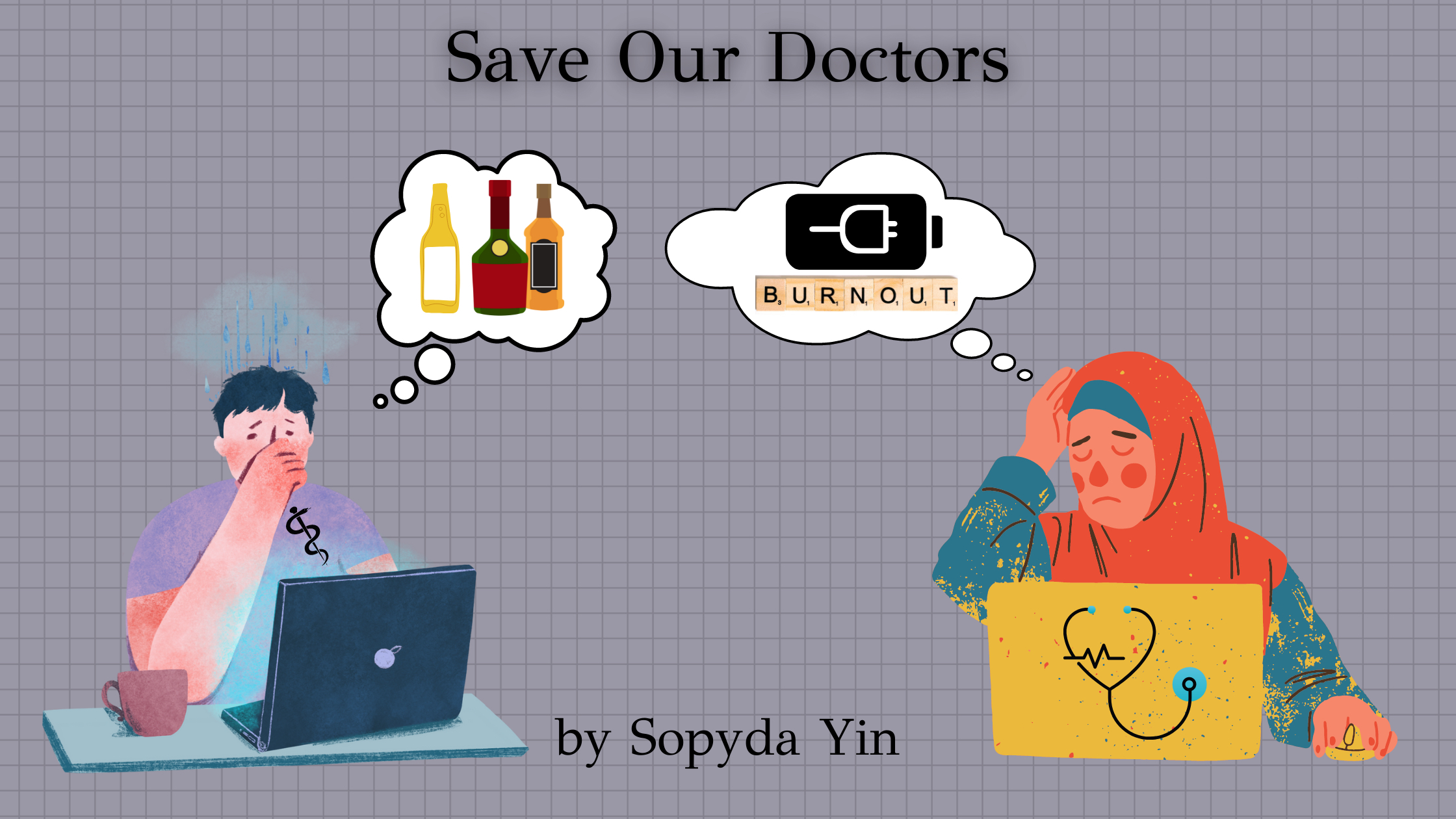
Physicians dedicate decades of training and education to provide life-saving treatments, cures, and groundbreaking research in healthcare. Even though they devote endless nights and calls to take care of their patients, many physicians often forget to reserve time for themselves, driving many to mental and physical exhaustion and burnout. While the COVID-19 pandemic has significantly overwhelmed physicians for the past two years, most physicians have experienced burnout before the pandemic. In the United States, roughly 300 to 400 physicians die by suicide annually. Male physicians have a suicide rate as high as 40%, while female physicians have as high as 130% greater than the general population.
Major risk factors for suicide include mental illness, emotional abuse, exhaustion, substance-use disorder, impaired relationship, and self-destructive tendency. For physicians, a significant factor in elevated depression and suicide risk is population-specific. Taking care and being responsible for a patient’s health is taxing. With the already increased physician shortage in the United States, physicians carry a heavy burden in their professional life to accommodate a growing population. Besides providing direct patient care, physicians’ work hours are further occupied with bureaucratic tasks like charting, insurance, and paperwork, which take a heavy toll on their personal life. Approximately 56% of physicians reported that burnout is likely due to bureaucracy, lack of respect and clinical autonomy, and increased use of EMR (electronic medical record). A study reported that during an examination, physicians consume 37% more interacting with the EMR than with their patients. For every patient interaction, a physician spends an additional two hours on the EMR at the clinic and another two hours during their personal time. Many physicians have addressed that feeling burnt out prevents them from spending time with their loved ones or resolving personal conflicts.
While physician burnout and suicide are common and damaging, it remains taboo in the workplace since stress management and suicide prevention are not accommodated properly during medical school and residency. In residency, most residents experience sleep deprivation, emotional abuse, toxic relationships with the program, and intensive work hour commitment. In a 2020 survey conducted by Medscape, physician burnout increased from 32% to 49%, and specialists with the highest burnout rate are in urology, neurology, internal medicine, and family medicine. The lack of support and care can explain why some physicians may turn to substance abuse like alcohol or depersonalize themselves to cope when distressed. In addition, research shows that burnout can drive physicians to develop compassion fatigue where they can feel disconnected from their patients, colleagues, and professional life.
Even though some workplaces offer wellness programs, many physicians may not participate in them for fear of disclosing their mental health. Others may believe that these programs are ineffective because the problem stems from the US healthcare system rather than physicians individually. While personal wellness like exercise and meditation can symptomatically improve burnout, the root cause will remain lasting if adequate reforms are not addressed and made. Physician burnout and suicide will lead to undesirable consequences including, but not limited to, lower patient satisfaction, higher medical error, malpractice risk, substance abuse, addiction, depression, and suicide. Reforming our healthcare system and destigmatizing mental health by providing professional services are needed to combat this ongoing crisis. We need to promote effective measures for healthcare workers to work in a safe environment. It is such a disservice to the ones saving lives who end up taking their own.









