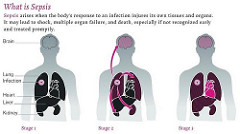
Sepsis is a three-stage disease that affects more than a million people each year in the United States with a mortality rate of 28% to 50%. Patients with weakened immune systems are especially vulnerable to developing the condition. The disease is caused by a massive immune response to infection, which causes many tiny blood clots that cause blood vessels to leak. This, in turn, inhibits the flow of fresh oxygen and nutrients to tissues. In the third stage of sepsis, blood pressure suddenly drops, leading to organ failure and death. Diagnosing sepsis is particularly difficult because its symptoms, like fevers, chills, and rapid heart rate, can also be caused by other diseases or complications. Furthermore, the symptoms of sepsis can develop at an unpredictable rate. According to Peter J. Pronovost, head of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins Medicine, “Right now, much of sepsis is invisible until someone is on death’s door.”
Image source: Dr. Gopal Murti
Current methods of diagnosis rely mostly on blood tests for abnormal numbers of white blood cells, which play a vital role in the immune system response, and testing bodily fluids for infection. Dr. Hagar at the Johns Hopkins Hospital teamed up with computer scientists also at Johns Hopkins to develop a more accurate and reliable method of metric for diagnosing sepsis. The team developed a computer algorithm that combined 27 of the most common measurements used to predict sepsis from over 16,000 patient electronic health records and compiled them into a “Targeted Real-time Warning Score,” or TREWScore. This metric was able to accurately predict 85% of patients at risk for septic shock faster and more accurately than another competing metric called the Modified Early Warning Score (MEWS). The system can be built into online health records systems to automatically alert physicians of at-risk patients. However, it would have to be integrated in a way to avoid causing “alarm fatigue“–desensitization of clinicians to alarms by many repeated false alarms. A clear distinction between low-risk and high-risk patients can minimize the potential for false alarms.
This computer system can help doctors make more accurate predictions for several other diseases such as, “acute lung injury, pneumonia, and post-rehabilitation illnesses like neuropathy” (Lauren J. Young, IEEE Spectrum).
Feature Image Source: Sepsis Awareness Poster Info by lynnmarentette