When people think of blood disorders, they tend to think about leukemia or hemophilia. Surprisingly enough, a less mainstream condition–thalassemia–is actually the most prevalent genetic blood disorder worldwide! Unlike leukemia, a cancer of the blood and bone marrow, and hemophilia, a condition where your blood fails to clot properly, thalassemia causes affected individuals to produce an abnormal form of hemoglobin, the protein instrumental in transporting oxygen. Hemoglobin is constructed of even portions of the proteins α-globin and β-globin. A defect in the genetic code that changes the production of either of these proteins can lead to thalassemia.
Different Types of Thalassemia
When discussing the different “types” of thalassemia, the distinctions indicate both the specific portion of hemoglobin that is affected and the severity of the disease. Alpha or beta thalassemia designate which portion of hemoglobin is deficient. Low alpha protein levels lead to α-thalassemia while low beta proteins levels lead to β-thalassemia.
Image Source: Donald Erickson
The severity is designated with the words “trait,” “minor,” “intermedia,” or “major.” An individual with thalassemia trait might show no symptoms. However, an individual with thalassemia major may have severe symptoms and require regular blood transfusions. These blood transfusions continually introduce large amounts of iron into an individual’s blood. Without an additional treatment, known as chelation therapy, the individual receiving these blood transfusions would literally rust to death due to iron overload.
Am I at Risk of Having Thalassemia?
Most individuals with severe thalassemia, like β-thalassemia major, discover their condition in childhood due to early abnormal anemia. Since thalassemia is genetically inherited, an individual can only inherit a severe form of thalassemia if both parents are carriers.
Thalassemia flourishes in areas where malaria is rampant, as it provides protection from malaria. Researchers believe that up to 40% of people in Africa, where malaria is one of the biggest killers, are trait carriers. Therefore, it’s highly recommended to be tested if one has family in these areas.
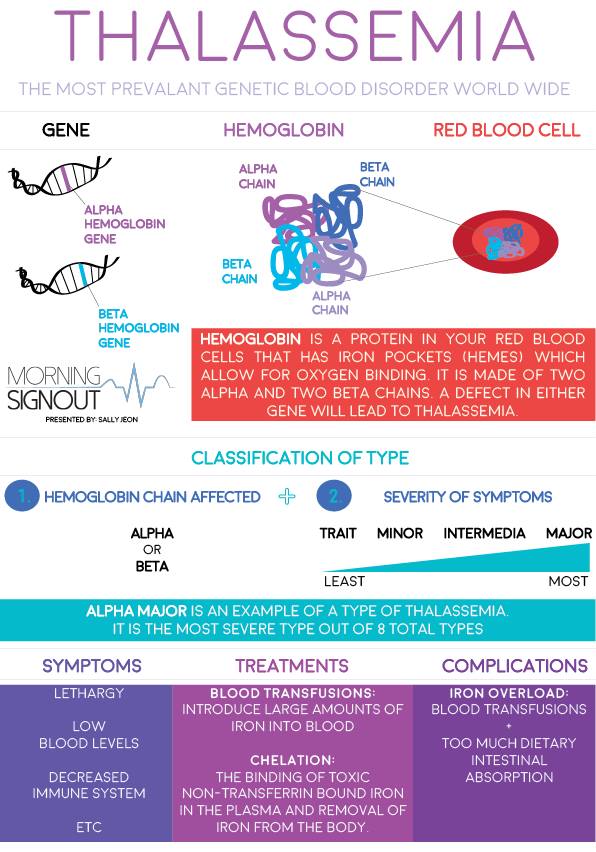
Here is a quick overview of Thalassemia. Source: Sally Jeon
Treatment Options
An individual’s physician will develop a personalized treatment plan to combat thalassemia. In general, treatment requires a combination of blood transfusions, bone marrow transplants, medications, and/or chelation therapy. Chelation is the process of removing excess iron and other heavy metals from the body after blood transfusions.
Whereas a diagnosis of thalassemia used to be terrifying, thalassemia is now a treatable condition. Many individuals with thalassemia go on to lead happy and healthy lives!
If you or a family member suspect that you have thalassemia, please consult with your doctor.
Featured Image Source: Wellcome Images