A recent case of antibiotic-resistant bacteria had the news media printing apocalyptic headlines. But what makes this such a historic medical case, and how does it affect us? First, we must start with the facts. The case involved a 49-year-old female in Pennsylvania with a urinary tract infection of the Escherichia coli (E. coli) bacteria. The bacteria was found to be resistant to the antibiotic colistin. Colistin is often used as a last resort for infections that have resisted all other antibiotics. Fortunately for the woman, she was able to be treated with another antibiotic and has fully recovered.
The big issue is not the fact that this bacteria was resistant to colistin; it is how it became resistant. The bacteria’s colistin-resistance gene was on a piece of DNA called a plasmid. Plasmids are easily and rapidly exchanged between bacteria, and the public health fear is that this resistant trait will spread rapidly. This is the first known case of plasmid colistin-resistant genes in America, and it most certainly is not the last we have seen of it.
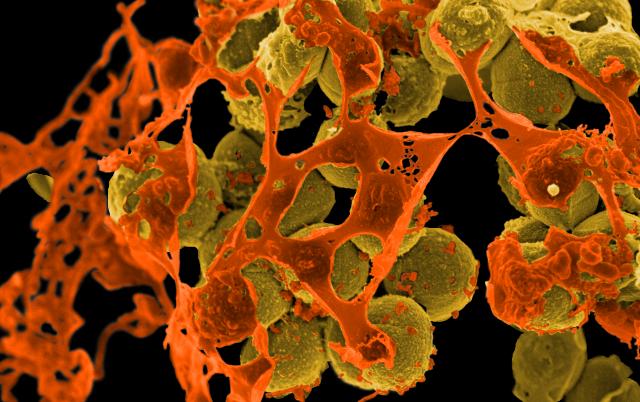
Image Source: Science Photo Library – SCIEPRO
Are we all in immediate danger? The general public is not in immediate danger of contracting an antibiotic-resistant bacteria. However, there are certain populations that are susceptible. For example, hospitals and facilities where groups of people are often prescribed a lot of antibiotics are at a greater risk for developing a resistant strain. People that have compromised immune systems, such as chemotherapy patients, have a higher susceptibility as well.
What can be done today? First, we must be diligent in our use of antibiotics. They should only be used to fight off bacterial infections and never viruses, such as the cold or flu. Even if every person on Earth followed this rule, bacteria will still find a way to develop resistance to the antibiotics. Bacteria have been on Earth much longer than humans and can mutate and adapt quickly to changing conditions. We must continue the development of new antibiotics to stay ahead of resistant bacteria. Currently, there is little incentive for pharmaceutical companies to spend money to develop new antibiotics. Antibiotics are cheap, so there is no monetary reward for the private development of a new antibiotic. If the private sector does not invest in this cause, the federal government has a responsibility to subsidize private development of new drugs.
Feature Image Source: Methicillin-Resistant Staphylococcus aureus (MRSA) Bacteria by NIAID