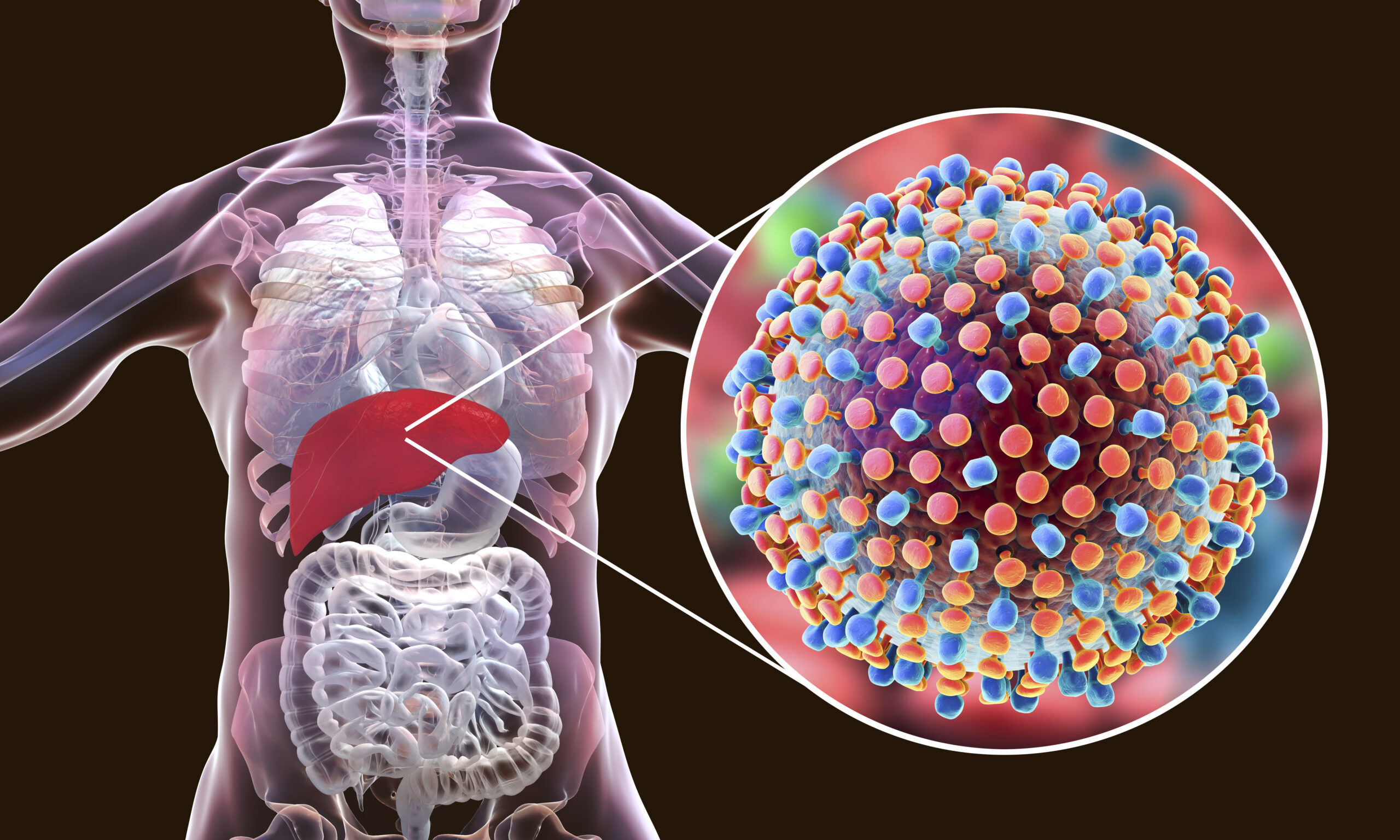
Hepatitis C is a deadly but silent disease. Experts believe that 4.1 million Americans previously lived with or are currently living with hepatitis C (HCV). It is a virus that spreads through the exposure of an infected person’s blood. People most at risk for having hepatitis C include those who share needles while using illicit drugs, healthcare workers who can get needlestick injuries, or anyone that has received either unsafe blood or clotting factor before testing and awareness became more widespread around 1990. Occasionally, people can become infected with hepatitis C by sharing personal hygiene items such as razors and toothbrushes or by having unprotected sex. Once hepatitis C enters the body, it targets the liver, causing swelling and damage. Sometimes, the body can get rid of hepatitis C on its own. However, upwards of every 3 out of four people infected with the virus will develop chronic hepatitis C, meaning they will not recover without treatment. Chronic hepatitis C can cause cirrhosis (liver scarring), liver cancer, other liver diseases, and, even, death.
Most people with hepatitis C don’t feel sick and don’t know they have it until they get tested. However, 20% to 30% of people with hepatitis experience an acute illness two weeks to six months after exposure. These acute symptoms include nausea, fatigue, body aches, abdominal pain, dark urine, clay colored feces, and yellowing of the eyes and skin. If the infection becomes chronic, people may experience symptoms of liver damage – including bleeding and bruising easily, itching, abdominal swelling, and confusion – in addition to the symptoms seen in acute hepatitis C. It is even possible for people with chronic hepatitis C not to feel sick even if their liver is damaged.
Since people infected with hepatitis C are often asymptomatic, or have no symptoms, hepatitis C often spreads without people knowing. The number of Americans diagnosed with hepatitis C has increased, with new cases per year jumping from approximately quadrupling from 2010 to 2017. The most at-risk group is people born between 55 and 75 years old. However, the infection rate in younger adults between the ages of 20 and 39 has increased because of intravenous drug use, direct injection into the veins. The United States Preventive Task Force now recommends that everyone between 18 and 79 should be tested for hepatitis C at least once during their lifetime. People who are at higher risk for contracting hepatitis, including those who use intravenous drugs like heroin, should be tested regularly.
A primary care provider can order a screening test for hepatitis C. Tests can be done at the provider’s office or local labs. This blood test looks for HCV antibodies, the protein the immune system makes while fighting an infection. If the HCV antibody is found in a blood sample, additional tests may be ordered to gauge liver damage and viral presence.
Image Source: Andrew Brookes
HCV is treated with a class of medications called direct-acting antivirals. These drugs work by stopping replication of the virus. 80% to 90% of people who complete their HCV treatment are cured.
To prevent infection, experts recommend wearing gloves while touching blood or open wounds, using sterile needles, practicing safe sex, and not sharing personal hygiene items. While there is no vaccine to prevent hepatitis C, you should follow these guidelines and consider getting tested at least once in your lifetime.
Featured Image Source: © Kateryna_Kon / Adobe Stock