Sickle cells form when hemoglobin, a protein found in RBCs that allows them to transport oxygen, is mutated. Normal RBCs have evenly spaced hemoglobin molecules, which allows RBCs to be flexible. Mutations can cause hemoglobin molecules to stick to each other and clump up on one side, forcing RBCs into a sickle-like shape. However, scientists have discovered that fetal RBCs express special fetal hemoglobin that doesn’t have the mutation to form sickle cells. This prompts the question: can producing fetal hemoglobin in “adult” RBCs allow for properly functioning blood cells?
Another protein called BCLIIa helps control the expression, or levels, of fetal hemoglobin in RBCs. As a fetus gets ready to be born, expression of BCLIIa increases, which lowers fetal hemoglobin expression and increases adult hemoglobin expression in RBCs. Interestingly, decreasing the levels of BCLIIa in adult RBCs can increase the expression of fetal hemoglobin, and in mice, can revert the blood cell shape to a disc-like shape and prevent symptoms of SCD from occurring.
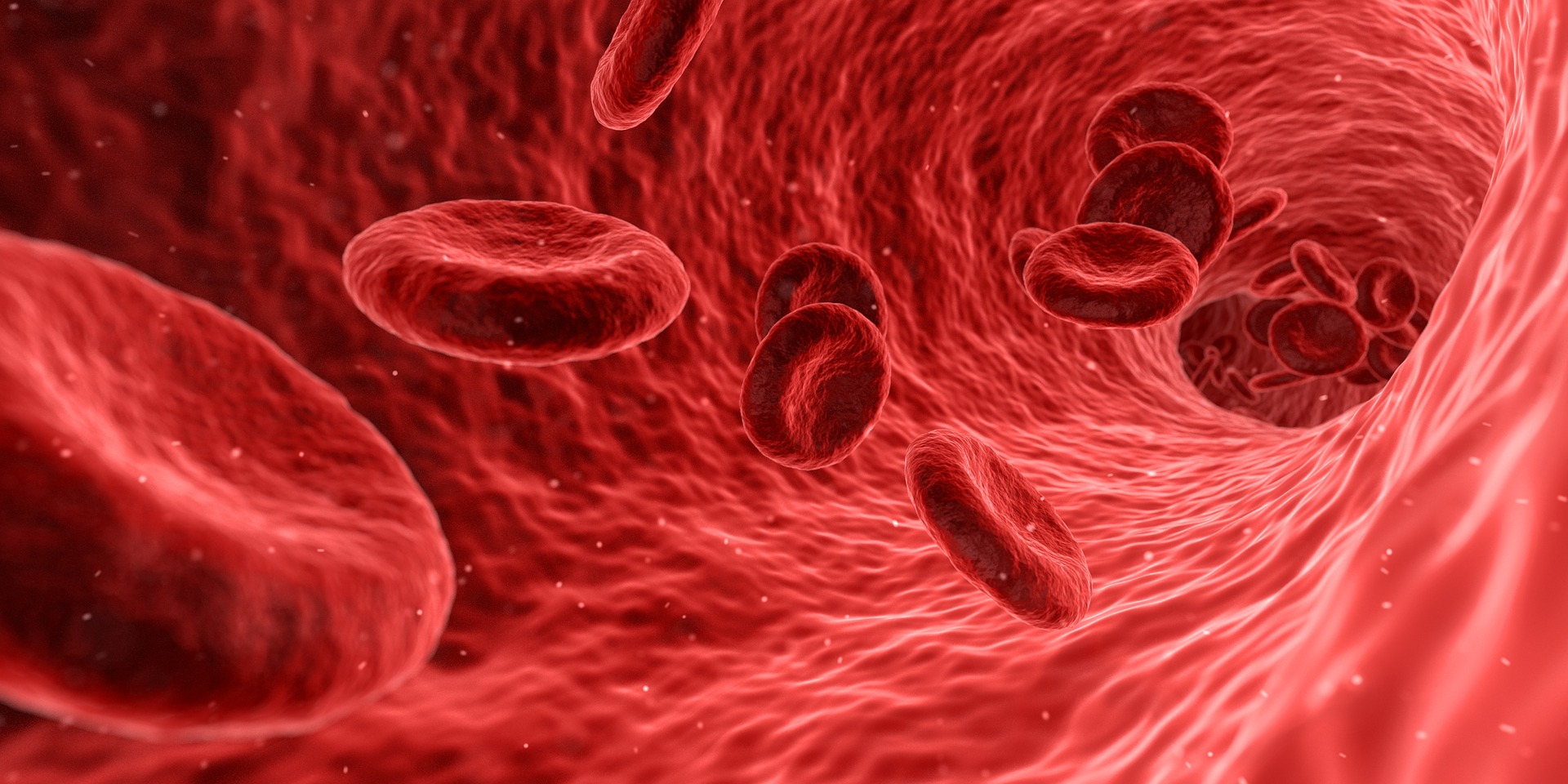
Image Source: Thana Prasongsin
A recent study by the Harvard Medical School utilized this knowledge to develop a “gene therapy” for humans that increases fetal hemoglobin in adult blood cells. To do this, scientists took hematopoietic stem cells (HSC), or cells that can turn into different blood cell types, from patients with severe SCD. Researchers then put in short hairpin RNAs (shRNA), molecules that can stop cells from making a certain protein, that would specifically lower levels of BCLIIa in HSCs. This would increase fetal hemoglobin levels, helping RBCs to take up their normal disc-like shape.
After transplantation of the edited stem cells back into patients, they were all shown to have increased concentrations of fetal hemoglobin and lower concentrations of mutated adult hemoglobin in their RBCs. In addition, after transplantation, patients required fewer blood transfusions, and there were little to no incidences of stroke or acute chest syndrome.
This study indicates that increasing levels of fetal hemoglobin in patients with SCD may be able to provide long-term relief. However, further studies should continue to test this method to ensure this treatment isn’t harmful in the long run. With more experiments and patience, SCD could someday be easily treated.
Featured Image Credit: SciTechTrend