The medical field was forever changed in the 20th century upon the discovery and increased usage of antibiotics, chemical agents used to kill or prevent the growth of bacteria. Disease-causing bacteria that have developed a resistance to antibiotics are a cause for major concern nowadays, but non-resistant bacteria, with the ability to promote the persistence of bacterial infections, additionally deserve our attention. A recent study provides evidence that non-resistant bacteria may be able to survive lethal concentrations of antibiotics through a density-dependent adaptive resistance mechanism. Concentration gradients of antibiotics facilitate the survival of these bacteria because antibiotics may penetrate only certain types of tissues in the body. Consequently, there are “safe spaces” for these bacteria to grow.
Image Source: Joe Raedle
Scientists studied the influence that these antibiotic gradients had on non-resistant bacteria. They connected two miniature compartments to allow for bacterial migration between the two. One compartment was continuously supplemented with Lysogeny broth (LB), a nutrient-rich liquid medium that promotes the growth of bacteria. The other compartment was continuously supplemented with LB containing a lethal dose of kanamycin, an antibiotic that disrupts protein synthesis within the cell. Diffusion of this antibiotic through the connection allowed for the development of a concentration gradient.
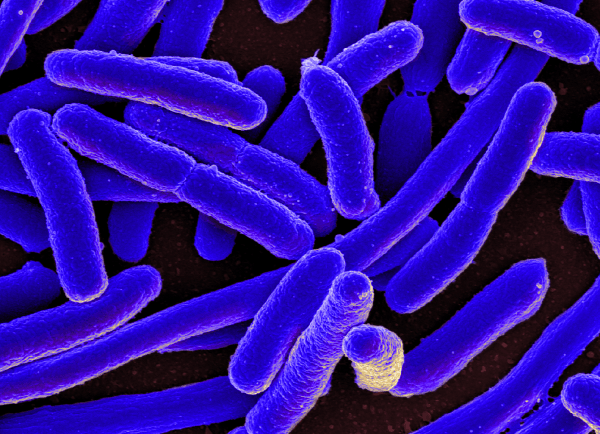
By inoculating fluorescently labeled Escherichia coli in the compartment containing no kanamycin, researchers visualized that these bacteria could swim into this antibiotic-free region, due to the presence of organelles called flagella, and colonize. Following this, researchers observed migrating “waves” of bacteria. These first “waves” of bacteria migrated to the compartment containing kanamycin but did not display growth. Over time, however, later population waves showed an increase in density. Surprisingly, these bacterial populations were able to survive and expand in the presence of the lethal dosage of kanamycin. These populations reached population densities comparable to bacterial populations thriving in antibiotic-free LB. Researchers measured the maximum local population density of the “waves” invading bacterial populations and found that successful colonization of the kanamycin compartment was dependent upon the population exceeding a critical baseline population density. Finally, researchers confirmed that the bacteria that were able to colonize the antibiotic compartment had the same sensitivity to kanamycin before and after the experiment, demonstrating that their ability to colonize the antibiotic compartment was not due to any form of genetically encoded resistance, but rather a type of phenotypic resistance.
With whole-genome sequencing, researchers found a resistant mutant, prompting the hypothesis that adaptive resistance may serve as a route for bacteria to acquire genetic resistance.
Feature Image Source: E. coli Bacteria by NIAID